Caloric restriction mimetics enhance anti-tumor efficacy

We’re happy to announce that the Seerave Fellow Dr. Jonathan Pol published part of his work entitled “A synergistic triad of chemotherapy, immune checkpoint inhibitors, and caloric restriction mimetics eradicates tumors in mice” in the journal OncoImmunology.
The lab of Professor Guido Kroemeber has recently shown that chemotherapy with agents inducing immunogenic cell death (ICD), such as anthracyclines (e.g. mitoxantrone) or the platinum salt oxaliplatin, can be advantageously combined with fasting or caloric restriction mimetics (CRMs) to reach a better control of tumor growth (1-3). The antitumor activity of the treatment depended on immune actors, particularly on CD8+ T cells. Among these CRMs, Jonathan Pol was particularly interested in further studying hydroxycitrate (HC) and spermidine (SPD). In this follow up study, Jonathan Pol and colleagues revealed that the myeloid immune compartment is also required for the efficacy of this therapeutic combination (4). Indeed, blocking of the integrin CD11b, which participates in the extravasation of myeloid cells, abrogated the benefit of CRMs to chemotherapy. In-depth characterization of the myeloid and lymphoid immune subpopulations infiltrated into the tumor bed allowed a better understanding of the underlying immune mechanisms. In particular, when combined with chemotherapy, HC and fasting amplified a population of dendritic cells derived from monocytes (moDCs, Ly6ChiLy6G+CD11c+CD11b+) and displaying an activated phenotype (CD80+MHC-IIint/hi). In contrast, complementation with SPD was responsible for an increased infiltration of inflammatory macrophages (F4/80+CD11b+CD11c–CD38+).
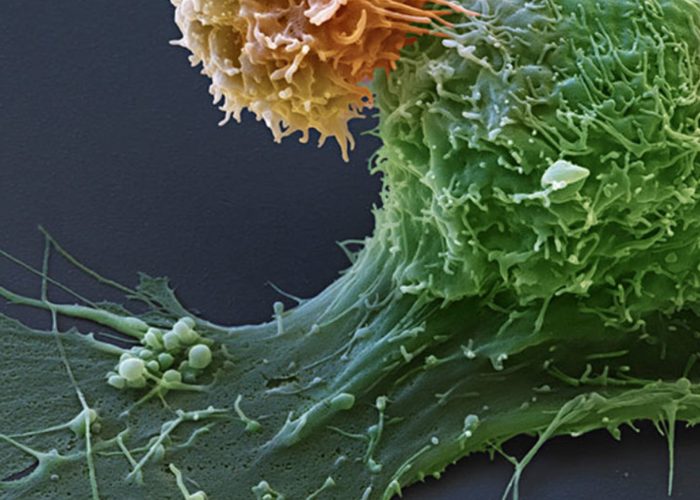
These moDCs and macrophages participate in cancer immunosurveillance by promoting the activation of CD8+ T lymphocytes able to eliminate malignant cells. Interestingly, chemotherapy alone doubled the influx of CD8+ T cells into the tumor. In combination with fasting, their infiltration was further increased but was accompanied by a more pronounced exhaustion phenotype, as shown by the expression of the negative immune feedback molecule PD-1 at the surface of CD8+ T cells. In comparison, the introduction of CRMs maintained a CD8+ T cell population of comparable size to chemotherapy alone but less exhausted than with fasting. In contrast, the CRM HC appeared to induce a rise in activated CD8+ T lymphocytes, characterized by the expression of the surface marker ICOS.
In parallel, Jonathan Pol and colleagues found that chemotherapy was inducing the overexpression of PD-L1 (PD-1 ligand) on both cancer cells and leukocytes (typically the myeloid compartment). Thus, the detection of PD-1 and PD-L1, both inhibiting the antitumor activity, on multiple cellular components of the tumor environment prompted us to introduce an immunotherapy blocking the PD-1/PD-L1 axis. The latter treatment relies on the administration of an antibody targeting PD-1 that prevents the interaction with its ligand PD-L1. Three anti-PD-1 immunotherapies are nowadays approved into the clinic: Nivolumab (Opdivo, BMS), Pembrolizumab (Keytruda, MSD), and Cemiplimab (REGN-2810, Sanofi). In our mouse fibrosarcoma model, treatment with anti-PD1 alone or in combination with fasting or CRMs had no significant antitumor effect. In contrast, the combination of anti-PD-1 with chemotherapy provided a benefit comparable to that of CRMs. However, complete regression of the majority of tumors was obtained only by a triple therapy combining (i) ICD-inducing chemotherapy, in this case mitoxantrone or oxaliplatin, (ii) a CRM such as HC or SPD, and substitutable by fasting, and (iii) an antibody blocking PD-1 and PD-L1 interaction. (4).
Overall, these results suggest the possibility of synergistic interactions between distinct classes of anticancer agents. Clinical trials are in preparation to evaluate this therapeutic triad against different malignant indications.
Full article: https://doi.org/10.1080/2162402X.2019.1657375
References:
- F. Pietrocola*, J. Pol*, E. Vacchelli, S. Rao, D. P. Enot, E. E. Baracco, S. Levesque, F. Castoldi, N. Jacquelot, T. Yamazaki, L. Senovilla, G. Marino, F. Aranda, S. Durand, V. Sica, A. Chery, S. Lachkar, V. Sigl, N. Bloy, A. Buque, S. Falzoni, B. Ryffel, L. Apetoh, F. Di Virgilio, F. Madeo, M. C. Maiuri, L. Zitvogel, B. Levine, J. M. Penninger, G. Kroemer, Caloric Restriction Mimetics Enhance Anticancer Immunosurveillance. Cancer Cell 30, 147-160 (2016).
- F. Pietrocola*, J. Pol* E. Vacchelli, E. E. Baracco, S. Levesque, F. Castoldi, M. C. Maiuri, F. Madeo, G. Kroemer, Autophagy induction for the treatment of cancer. Autophagy 12, 1962-1964 (2016).
- F. Pietrocola*, J. Pol*, G. Kroemer, Fasting improves anticancer immunosurveillance via autophagy induction in malignant cells. Cell Cycle 15, 3327-3328 (2016).
- S. Levesque, J. Le Naour, F. Pietrocola, J. Paillet, M. Kremer, F. Castoldi, E. E. Baracco, Y. Wang, E. Vacchelli, G. Stoll, A. Jolly, P. De La Grange, L. Zitvogel, G. Kroemer, J. G. Pol, A synergistic triad of chemotherapy, immune checkpoint inhibitors, and caloric restriction mimetics eradicates tumors in mice. Oncoimmunology 8, e1657375 (2019).
Continue Reading